SUMMARY: The American Cancer Society estimates that in 2014, 18,860 new cases of Acute Myeloid Leukemia (AML) will be diagnosed in the United States and 10,460 patients will die of the disease. Acute Myeloid Leukemia in general is a disease of the elderly and the average age of a patient with AML is about 66 years. AML can be considered as a group of heterogeneous diseases with different clinical behavior and outcomes. Cytogenetic analysis has been part of routine evaluation when caring for patients with AML. By predicting resistance to therapy, tumor cytogenetics will stratify patients, based on risk and help manage them accordingly. Even though cytotoxic chemotherapy may lead to long term remission and cure in a minority of patients with favorable cytogenetics, patients with high risk features such as unfavorable cytogenetics, molecular abnormalities, prior myelodysplasia and advanced age, have poor outcomes with conventional chemotherapy.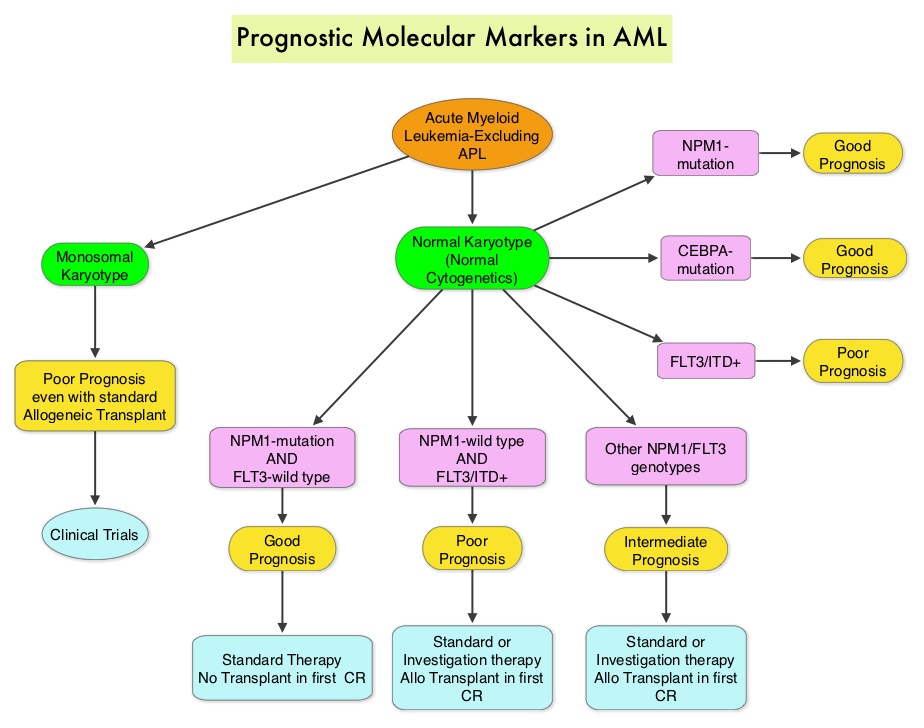 The Fms-Like Tyrosine kinase 3 (FLT3) is a receptor tyrosine kinase in the PDGF family of growth factor receptors located on the cell surface (transmembrane) and plays an important role in both normal and malignant hematopoiesis by activating key signaling pathways. Activating mutations in the FLT3 receptor is the most common genetic abnormality in AML and is detected in approximately 30% of the patients. The most common FLT3 mutation is the FLT3-ITD (Internal Tandem Duplication) mutation caused by tandem duplication within the coding region of the gene. The presence of FLT3-ITD mutations can negate the benefit of any other favorable molecular and cytogenetic features. Patients with FLT3-ITD mutations are predicted to have poor outcomes with shorter remission duration and significantly decreased leukemia free and overall survival. These mutations are detected using Polymerase Chain Reaction (PCR) based molecular diagnostic DNA testing. The authors in this meta-analysis examined the prognostic significance of three mutations frequently noted in patients with cytogenetically normal Acute Myeloid Leukemia. These mutations included FLT3-ITD, mutated NPM1 (Nucleophosmin) and mutations of the CCAAT enhancer-binding protein alpha (CEBPA) gene. This systematic review and meta-analysis included 1942 patients from multiple electronic databases from 2000 to March 2012. It was noted that FLT3-ITD was associated with the worse prognosis, with inferior Overall Survival (OS) and Relapse Free Survival (RFS), whereas mutations in NPM1 and CEBPA genes were associated with a favorable prognosis. The discovery of new molecular mutations in AML patients with normal cytogenetics may help predict outcomes and provide valuable information to facilitate risk-adapted therapy. Port M, Böttcher M, Thol F, et al. Ann Hematol. 2014;93:1279-1286
The Fms-Like Tyrosine kinase 3 (FLT3) is a receptor tyrosine kinase in the PDGF family of growth factor receptors located on the cell surface (transmembrane) and plays an important role in both normal and malignant hematopoiesis by activating key signaling pathways. Activating mutations in the FLT3 receptor is the most common genetic abnormality in AML and is detected in approximately 30% of the patients. The most common FLT3 mutation is the FLT3-ITD (Internal Tandem Duplication) mutation caused by tandem duplication within the coding region of the gene. The presence of FLT3-ITD mutations can negate the benefit of any other favorable molecular and cytogenetic features. Patients with FLT3-ITD mutations are predicted to have poor outcomes with shorter remission duration and significantly decreased leukemia free and overall survival. These mutations are detected using Polymerase Chain Reaction (PCR) based molecular diagnostic DNA testing. The authors in this meta-analysis examined the prognostic significance of three mutations frequently noted in patients with cytogenetically normal Acute Myeloid Leukemia. These mutations included FLT3-ITD, mutated NPM1 (Nucleophosmin) and mutations of the CCAAT enhancer-binding protein alpha (CEBPA) gene. This systematic review and meta-analysis included 1942 patients from multiple electronic databases from 2000 to March 2012. It was noted that FLT3-ITD was associated with the worse prognosis, with inferior Overall Survival (OS) and Relapse Free Survival (RFS), whereas mutations in NPM1 and CEBPA genes were associated with a favorable prognosis. The discovery of new molecular mutations in AML patients with normal cytogenetics may help predict outcomes and provide valuable information to facilitate risk-adapted therapy. Port M, Böttcher M, Thol F, et al. Ann Hematol. 2014;93:1279-1286

