SUMMARY: The National Comprehensive Cancer Network (NCCN) has expanded its Survivorship Guidelines to include cancer-associated cognitive impairment and Chemotherapy Induced Peripheral Neuropathy. The later is a component of the Adult Cancer Pain section. Dr. Urba discussed the management of Chemotherapy Induced Peripheral Neuropathy at the NCCN 19th annual conference. Approximately 20%-40% of the patients suffer from Chemotherapy Induced Peripheral Neuropathy, which can result in premature discontinuation of treatment. Further, this adverse event in a significant number of patients can persist indefinitely and can be disabling, thus impacting their activities of daily living. The following chemotherapeutic agents are associated with varying degrees of peripheral neuropathy – Platinum compounds (Cisplatin, Carboplatin and Oxaliplatin), Taxanes (Paclitaxel, Docetaxel), Immunomodulatory agents (Thalidomide, Lenalidomide), Other Microtubule inhibitors (Vincristine, Ixabepilone) and Proteosome Inhibitors (Bortezomib). It may be necessary to screen and rescreen patients for neuropathic pain, as patients may not be forthcoming with this complaint. Management of Neuropathic pain may include systemic treatment with adjuvant analgesics, topical therapies and psychosocial support. The management of Chemotherapy Induced Peripheral Neuropathy has mostly been extrapolated from validated studies on diabetic neuropathy. The first line treatment for Chemotherapy Induced Neuropathic Pain includes antidepressants and anticonvulsants, which if not effective on their own, can be combined with opioids. TriCyclic Antidepressants (TCA’s) such as Amitriptyline and Nortriptyline (PAMELOR®) can be considered as first line choice for appropriate patients, although its mechanism of action is uncertain and 20% of the patients discontinue therapy because of adverse effects.
The following chemotherapeutic agents are associated with varying degrees of peripheral neuropathy – Platinum compounds (Cisplatin, Carboplatin and Oxaliplatin), Taxanes (Paclitaxel, Docetaxel), Immunomodulatory agents (Thalidomide, Lenalidomide), Other Microtubule inhibitors (Vincristine, Ixabepilone) and Proteosome Inhibitors (Bortezomib). It may be necessary to screen and rescreen patients for neuropathic pain, as patients may not be forthcoming with this complaint. Management of Neuropathic pain may include systemic treatment with adjuvant analgesics, topical therapies and psychosocial support. The management of Chemotherapy Induced Peripheral Neuropathy has mostly been extrapolated from validated studies on diabetic neuropathy. The first line treatment for Chemotherapy Induced Neuropathic Pain includes antidepressants and anticonvulsants, which if not effective on their own, can be combined with opioids. TriCyclic Antidepressants (TCA’s) such as Amitriptyline and Nortriptyline (PAMELOR®) can be considered as first line choice for appropriate patients, although its mechanism of action is uncertain and 20% of the patients discontinue therapy because of adverse effects.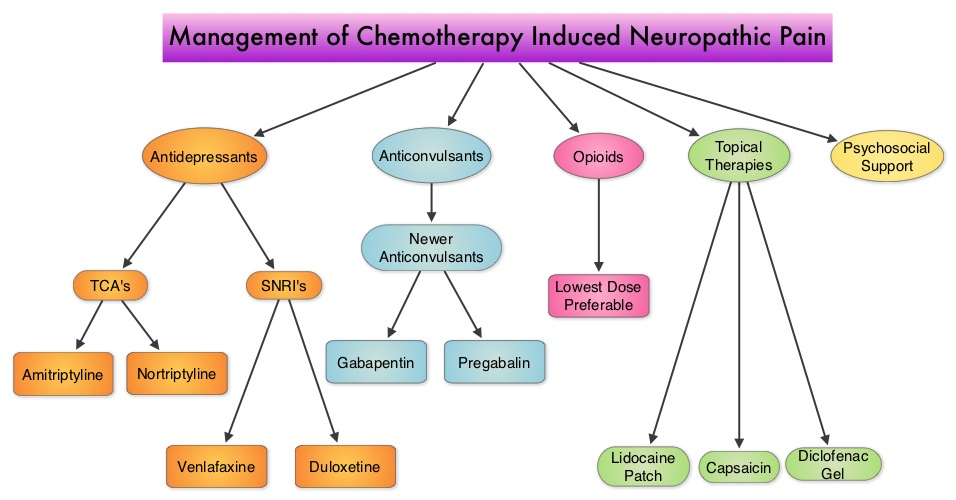 Patients may be able to better tolerate these agents if started at a lower dose and dose titrated slowly every three to five days. Peripheral neuropathic pain has been attributed to an unbalanced release of norepinephrine and serotonin from the neurons. Serotonin-Norepinephrine Reuptake Inhibitors (SNRI’s), including Venlafaxine (EFFEXOR®) and Duloxetine (CYMBALTA®), are better tolerated and have fewer drug interactions than TCA’s. EFFEXOR® in one study significantly relieved Oxaliplatin induced neuropathic pain in more than two thirds of the patients when compared to placebo and a third of the patients had complete pain relief. There is however limited evidence showing a beneficial role of Selective Serotonin Reuptake Inhibitors (SSRI’s) such as Citalopram (CELEXA®) and Paroxetine (PAXIL®) for neuropathic pain. As a note of caution, SNRI’s such as EFFEXOR® and CYMBALTA®, can interact with Tamoxifen, prescribed to patients with breast cancer, preventing Tamoxifen from converting to its active form. The dose of antidepressants needed to alleviate neuropathic pain is not dependent on antidepressant activity and may be lower than that recommended for treatment of depression. The newer anticonvulsants such as Gabapentin (NEURONTIN®), Pregabalin (LYRICA®) are preferable first line agents for the treatment of neuropathic pain rather than traditional, older agents such as Carbamazepine (TEGRETOL®), Phenytoin (DILANTIN®) and Valproate (DEPAKOTE®), as the newer agents are associated with fewer drug interactions. The newer agents bind to the alpha2-delta subunit of the calcium-sensitive channels, modulating neurotransmitter release. Of the newer agents, NEURONTIN® (Gabapentin) is not protein bound and is excreted unchanged in the urine and therefore has fewer drug interactions. If opioids are a consideration for neuropathic pain relief, the lowest dose is recommended. Topical therapies for neuropathic pain have the advantage of controlling pain without systemic side effects. It therefore can be combined with systemic treatment. Lidocaine 5% patches (LIDODERM®) block neuronal sodium channels whereas Capsaicin cream (ZOSTRIX®) stimulates the C fibers to release and subsequently deplete substance P, there by blocking pain signaling to the brain. Diclofenac gel 1% when applied once a day, concentrates in the dermis and has less gastrointestinal side effects and may be beneficial for neuropathic pain. A combination of Ketamine 1% and Amitriptyline 2% cream applied topically has also been promising in a small study. Patients experiencing refractory pain may benefit with the use of Transcutaneous Electrical Nerve Stimulation (TENS), although referral to the pain clinic may be appropriate. Psychosocial support utilizing a team of specialists and social workers/counsellors, should be an integral part of pain management. Kvale E and Urba SG. National Comprehensive Cancer Network (NCCN) 19th Annual Conference, March 13 – 15, 2014; Hollywood, Florida
Patients may be able to better tolerate these agents if started at a lower dose and dose titrated slowly every three to five days. Peripheral neuropathic pain has been attributed to an unbalanced release of norepinephrine and serotonin from the neurons. Serotonin-Norepinephrine Reuptake Inhibitors (SNRI’s), including Venlafaxine (EFFEXOR®) and Duloxetine (CYMBALTA®), are better tolerated and have fewer drug interactions than TCA’s. EFFEXOR® in one study significantly relieved Oxaliplatin induced neuropathic pain in more than two thirds of the patients when compared to placebo and a third of the patients had complete pain relief. There is however limited evidence showing a beneficial role of Selective Serotonin Reuptake Inhibitors (SSRI’s) such as Citalopram (CELEXA®) and Paroxetine (PAXIL®) for neuropathic pain. As a note of caution, SNRI’s such as EFFEXOR® and CYMBALTA®, can interact with Tamoxifen, prescribed to patients with breast cancer, preventing Tamoxifen from converting to its active form. The dose of antidepressants needed to alleviate neuropathic pain is not dependent on antidepressant activity and may be lower than that recommended for treatment of depression. The newer anticonvulsants such as Gabapentin (NEURONTIN®), Pregabalin (LYRICA®) are preferable first line agents for the treatment of neuropathic pain rather than traditional, older agents such as Carbamazepine (TEGRETOL®), Phenytoin (DILANTIN®) and Valproate (DEPAKOTE®), as the newer agents are associated with fewer drug interactions. The newer agents bind to the alpha2-delta subunit of the calcium-sensitive channels, modulating neurotransmitter release. Of the newer agents, NEURONTIN® (Gabapentin) is not protein bound and is excreted unchanged in the urine and therefore has fewer drug interactions. If opioids are a consideration for neuropathic pain relief, the lowest dose is recommended. Topical therapies for neuropathic pain have the advantage of controlling pain without systemic side effects. It therefore can be combined with systemic treatment. Lidocaine 5% patches (LIDODERM®) block neuronal sodium channels whereas Capsaicin cream (ZOSTRIX®) stimulates the C fibers to release and subsequently deplete substance P, there by blocking pain signaling to the brain. Diclofenac gel 1% when applied once a day, concentrates in the dermis and has less gastrointestinal side effects and may be beneficial for neuropathic pain. A combination of Ketamine 1% and Amitriptyline 2% cream applied topically has also been promising in a small study. Patients experiencing refractory pain may benefit with the use of Transcutaneous Electrical Nerve Stimulation (TENS), although referral to the pain clinic may be appropriate. Psychosocial support utilizing a team of specialists and social workers/counsellors, should be an integral part of pain management. Kvale E and Urba SG. National Comprehensive Cancer Network (NCCN) 19th Annual Conference, March 13 – 15, 2014; Hollywood, Florida

