SUMMARY: According to the CIBMTR (Center for International Blood and Marrow Transplant Research), in 2012, over 11,000 Hematopoietic Stem Cell Transplants (HSCT) in the US were Autologous and over 7500 were Allogeneic. Multiple myeloma and Lymphoma accounted for 57% of all HSCTs and AML and Myelodysplasia accounted for 51% of Allogeneic HSCTs. There has been an increase in the number of Autologous and Allogeneic transplants for treatment of malignant diseases in elderly patients, with 39% of Autologous transplant recipients and 17% of Allogeneic transplant recipients between 2006-2012 reported to be older than 60 years of age. With increase in the number of long term survivors following transplantation, early and late complications of HSCT have been the focus of increasing attention.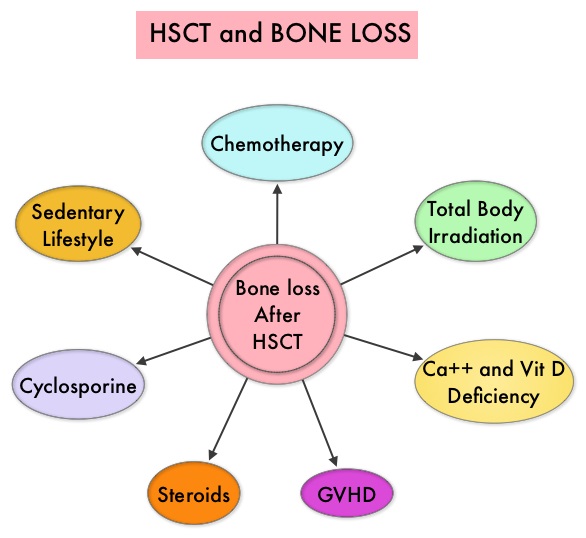 Morbidity and mortality as well as quality of life related to bone loss among long term survivors after HSCT, has been previously published. Factors contributing to bone loss in this patient population include intensive chemotherapy, total body irradiation, post-transplantation glucocorticoid use, reduced intake and metabolism of Calcium and Vitamin D, graft versus host disease, use of Cyclosporine-A and sedentary lifestyle after transplantation. Loss of Bone Mineral Density (BMD) occurs within 6 to 12 months after transplantation at all skeletal sites, followed by initial recovery of BMD in the lumbar spine and a slower recovery of BMD in the femur neck. This bone loss may persist for 48 to 120 months or even longer. The authors in this single institution, retrospective study, calculated the cumulative incidence rates of fractures among survivors of Autologous and Allogeneic Hematopoietic Stem Cell Transplantations (HSCT) and compared the rate of fractures to that of the general US population. Data was collected from 7,620 patients over 18 years of age who underwent HSCT at The University of Texas MD Anderson Cancer Center, from January 1997 to December 2011 and these patients were observed through December 2013. The authors then calculated the cumulative incidence of fractures, with death as a competing risk and the age and sex-specific fracture incidence rates were compared with those in the US general population, using estimated rates from the 1994 National Health Interview Survey and the 2004 National Hospital Discharge Survey. Of the 7,620 patients who underwent HSCT, 56% were male and 51% underwent Autologous and 49% underwent Allogeneic stem cell transplantation.
Morbidity and mortality as well as quality of life related to bone loss among long term survivors after HSCT, has been previously published. Factors contributing to bone loss in this patient population include intensive chemotherapy, total body irradiation, post-transplantation glucocorticoid use, reduced intake and metabolism of Calcium and Vitamin D, graft versus host disease, use of Cyclosporine-A and sedentary lifestyle after transplantation. Loss of Bone Mineral Density (BMD) occurs within 6 to 12 months after transplantation at all skeletal sites, followed by initial recovery of BMD in the lumbar spine and a slower recovery of BMD in the femur neck. This bone loss may persist for 48 to 120 months or even longer. The authors in this single institution, retrospective study, calculated the cumulative incidence rates of fractures among survivors of Autologous and Allogeneic Hematopoietic Stem Cell Transplantations (HSCT) and compared the rate of fractures to that of the general US population. Data was collected from 7,620 patients over 18 years of age who underwent HSCT at The University of Texas MD Anderson Cancer Center, from January 1997 to December 2011 and these patients were observed through December 2013. The authors then calculated the cumulative incidence of fractures, with death as a competing risk and the age and sex-specific fracture incidence rates were compared with those in the US general population, using estimated rates from the 1994 National Health Interview Survey and the 2004 National Hospital Discharge Survey. Of the 7,620 patients who underwent HSCT, 56% were male and 51% underwent Autologous and 49% underwent Allogeneic stem cell transplantation.  The most common reasons for HSCT were hematologic malignancies other than Multiple Myeloma (67%), Multiple Myeloma (22%) and other solid tumors (11%). The median follow up was 85 months. Fractures occurred in 8% of patients (N = 602) of whom 419 patients had an Autologous stem cell transplantation and 183 patients had Allogeneic stem cell transplantation. The incidence of fracture was higher in patients older than age 50 years, 5 times higher among patients with Multiple Myeloma compared to other hematologic malignancies and patients who underwent Autologous transplantation were 45% more likely to develop a fracture than those who underwent an Allogeneic transplantation. When age- and sex-specific fracture incidence rates after HSCT were compared with National Health Interview Survey data, females were at approximately 8 times greater risk and men 45-64 years old were at approximately 7-9 times greater risk of sustaining a fracture. The authors concluded that the incidence of fractures after HSCT is significantly higher and all patients undergoing HSCT should be considered to be at risk for post-transplantation bone loss. Measures to prevent bone loss and fractures include physical exercise, Vitamin D and Calcium supplementation, avoiding tobacco products, abstaining from excess alcohol intake and fall prevention. The authors recommend that patients undergoing HSCT should have a Dual Energy X-ray Absorptiometry scan performed at baseline and at 6 months following transplantation. Increased Incidence of Fractures in Recipients of Hematopoietic Stem-Cell Transplantation. Pundole XN, Barbo AG, Lin H, et al. J Clin Oncol 2015; 33:1364-1370
The most common reasons for HSCT were hematologic malignancies other than Multiple Myeloma (67%), Multiple Myeloma (22%) and other solid tumors (11%). The median follow up was 85 months. Fractures occurred in 8% of patients (N = 602) of whom 419 patients had an Autologous stem cell transplantation and 183 patients had Allogeneic stem cell transplantation. The incidence of fracture was higher in patients older than age 50 years, 5 times higher among patients with Multiple Myeloma compared to other hematologic malignancies and patients who underwent Autologous transplantation were 45% more likely to develop a fracture than those who underwent an Allogeneic transplantation. When age- and sex-specific fracture incidence rates after HSCT were compared with National Health Interview Survey data, females were at approximately 8 times greater risk and men 45-64 years old were at approximately 7-9 times greater risk of sustaining a fracture. The authors concluded that the incidence of fractures after HSCT is significantly higher and all patients undergoing HSCT should be considered to be at risk for post-transplantation bone loss. Measures to prevent bone loss and fractures include physical exercise, Vitamin D and Calcium supplementation, avoiding tobacco products, abstaining from excess alcohol intake and fall prevention. The authors recommend that patients undergoing HSCT should have a Dual Energy X-ray Absorptiometry scan performed at baseline and at 6 months following transplantation. Increased Incidence of Fractures in Recipients of Hematopoietic Stem-Cell Transplantation. Pundole XN, Barbo AG, Lin H, et al. J Clin Oncol 2015; 33:1364-1370

