SUMMARY: Multiple Myeloma is a clonal disorder of plasma cells in the bone marrow and the American Cancer Society estimates that in the United States, 34,920 new cases will be diagnosed in 2021 and 12,410 patients are expected to die of the disease. Multiple Myeloma (MM) in 2021 remains an incurable disease. The therapeutic goal therefore is to improve Progression Free Survival (PFS) and Overall Survival (OS). Multiple Myeloma is a disease of the elderly, with a median age at diagnosis of 69 years and characterized by intrinsic clonal heterogeneity. Almost all patients eventually will relapse, and patients with a high-risk cytogenetic profile, extramedullary disease or refractory disease have the worst outcomes. The median survival for patients with myeloma is over 10 years.
REVLIMID® (Lenalidomide) based regimens are often prescribed for patients with newly diagnosed, transplant-ineligible Multiple Myeloma. REVLIMID®, a thalidomide analogue has immunomodulatory, tumoricidal, and antiangiogenic properties, and synergizes with Dexamethasone to enhance anti-myeloma activity. DARZALEX® is a human IgG1 antibody that targets CD38, a transmembrane glycoprotein abundantly expressed on malignant plasma cells and with low levels of expression on normal lymphoid and myeloid cells. DARZALEX® exerts its cytotoxic effect on myeloma cells by multiple mechanisms, including Antibody Dependent Cellular Cytotoxicity (ADCC), Complement Mediated Cytotoxicity and direct apoptosis. Additionally, DARZALEX® may have a role in immunomodulation by depleting CD38-positive regulator Immune suppressor cells, and thereby expanding T cells, in patients responding to therapy. DARZALEX® has activity as both a single agent and when combined with other standard regimens. The primary analyses of several Phase III studies (ALCYONE, MAIA, and CASSIOPEIA) demonstrated superior clinical efficacy of DARZALEX® in combination with standard-of-care regimens, compared to standard of care alone, for patients with newly diagnosed multiple myeloma. The MAIA study compared the efficacy and safety of DARZALEX® plus REVLIMID® and Dexamathasone (D-Rd) with REVLIMID® and Dexamathasone (Rd), in transplant-ineligible newly diagnosed Multiple Myeloma patients.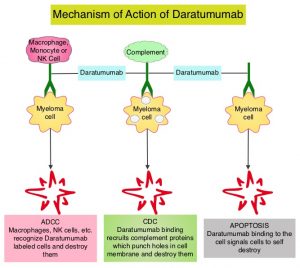
The MAIA study is a multicenter, international, open-label, phase III trial, which included 737 newly diagnosed Myeloma patients who were not candidates for high-dose chemotherapy and Autologous Stem Cell Transplant (ASCT), due to age 65 years or older or comorbidities. Patients were randomly assigned 1:1 to receive REVLIMID® 25 mg orally on days 1-21 of each 28-day cycle and Dexamethasone 40 mg once a week, with or without DARZALEX®. Patients assigned DARZALEX® (D-Rd regimen) received 16 mg/kg weekly for the first 8 weeks (cycles 1 and 2), every other week for 16 weeks (cycles 3 to 6), and then every 4 weeks (cycle 7 and beyond) until disease progression or unacceptable toxicity. Treatment groups were well balanced. The median patient age was 73 years, 99% of patients were 65 years or older and 44% of patients were 75-90 years old. Cytogenetic risk level could be determined in 642 patients of the total population. Eighty-six percent (86%) of these patients were standard risk and 14% were considered high risk. The Primary end point was Progression Free Survival (PFS). Key Secondary endpoints included Overall Survival (OS), Overall Response Rate (ORR), Minimal Residual Disease (MRD) negativity rate (10-5 sensitivity), and Safety.
In the primary analysis of the MAIA trial, D-Rd regimen reduced the risk of disease progression or death by 44%, compared to Rd. The authors now reported the updated efficacy and safety of D-Rd, compared to Rd, after almost 5 years of median follow up, in transplant-ineligible newly diagnosed Multiple Myeloma patients, from the prespecified interim OS analysis of MAIA.
After a median follow up of almost 5 years (56.2 months), the median OS was not reached (NR) in either treatment groups. The estimated 5-year OS rate was 66.3% with D-Rd and 53.1% with Rd (HR=0.68; P=0.0013). D-Rd reduced the risk of death by 32%. The updated median PFS was Not Reached with D-Rd versus 34.4 months with Rd. The estimated 5-year PFS rate was 52.5% with D-Rd and 28.7% with Rd (HR=0.53; P<0.0001). D-Rd reduced the risk of disease progression or death was reduced by 47%. The updated ORR was 92.9% with D-Rd versus 81.6% with Rd (P<0.0001).
The authors concluded that after almost 5 years of follow-up, the addition of DARZALEX® to REVLIMID® and Dexamethasone resulted in a significant improvement in Overall Survival, as well as significant reduction in the risk of disease progression or death, in newly diagnosed Multiple Myeloma patients, who are transplant-ineligible. The authors added that these results are more meaningful and support D-Rd as a new standard of care for this patient group, as this study population of elderly patients, never receive subsequent therapy.
OVERALL SURVIVAL RESULTS WITH DARATUMUMAB, LENALIDOMIDE, AND DEXAMETHASONE VERSUS LENALIDOMIDE AND DEXAMETHASONE IN TRANSPLANT-INELIGIBLE NEWLY DIAGNOSED MULTIPLE MYELOMA: PHASE 3 MAIA STUDY. Facon T, Kumar SK, Plesner T, et al. Presented at: European Hematology Association Annual Meeting; June 9-17, 2021; Virtual. Abstract LB1901.

