SUMMARY:The American Cancer Society's estimates that approximately 15,720 new cases of chronic lymphocytic leukemia (CLL) will be diagnosed in 2014 and approximately 4600 patients will die from the disease. CLL is a heterogeneous disease with a clinical course that is variable, with a very indolent course in some patients and some with aggressive disease and others somewhere in between. Both Binet and the Rai CLL staging systems developed in the 1970’s rely solely on physical examination and standard laboratory testing to predict survival. With the development of Interphase Fluorescent In Situ Hybridization (FISH) technique, which allows detection of genetic abnormalities in noncycling CLL cells, it has become clear that cytogenetic abnormalities are often seen in CLL patients and these genetic abnormalities in turn appear to be reliable predictors of disease progression, response to therapy and survival. Some of these cytogenetic abnormalities include del(13q), normal karyotype, trisomy(12), del(11q), del(17p), and they are associated with decreasing survival times, in that order. Another important prognostic factor is the rearrangement and somatic hypermutation of the variable region of the immunoglobulin heavy chain genes (IGHV), which is an independent predictor of outcome in CLL.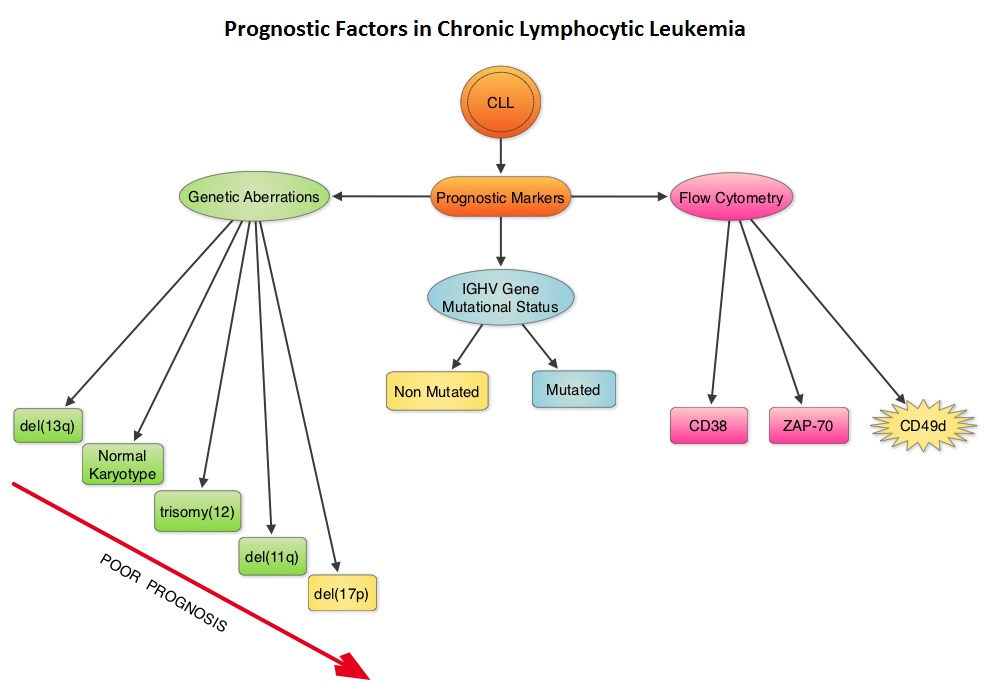 Retrospective studies have suggested that patients with CLL whose leukemic cells have clonotypically rearranged immunoglobulin genes in germline configuration (Unmutated IGHV gene) demonstrated more aggressive disease and shorter survival time compared to those patients with somatic hypermutations in their IGHV genes (Mutated IGHV gene). Expression of two flow cytometry based biomarkers, CD38 (surface marker) and ZAP-70 (intracytoplasmic protein), have been associated with poor outcomes. As we learn more about the pathobiology of CLL, it is becoming clear that survival of CLL cells is dependent not only on their intracellular defects but also on the microenvironment. CD49d, an integrin, is a surface molecule, detected by flow cytometry. CD49d expression promotes microenvironment mediated proliferation of CLL cells and has been associated with shortened survival. The authors conducted this multicenter analysis to evaluate the prognostic utility of CD49d in CLL, in comparison with CD38 and ZAP-70. The authors analysed the data of 2972 patients from 9 clinical trials. All these studies had data on CD49d expression of CLL cells by flow cytometry and reported the association between CD49d expression and Overall survival and/or Treatment Free Survival and/or Progression Free Survival. Patients with 30% or more of CLL cells expressing CD49d were considered CD49d positive. In this pooled analysis, CD49d positive patients had a significantly lower Overall Survival both at 5 years (87% vs 94%) and 10 years (62% vs 84%) compared with CD49d negative patients (P<0.001). Further, CD49d positive patients more likely required treatment, suggesting that these patients had a lower probability of remaining treatment free at both 5 years (42% vs 68%) and 10 years (24% vs 50%), compared with CD49d negative patients. When other variables were taken into consideration, CD49d was the only flow cytometry based marker which independently predicted Overall Survival with greater prognostic relevance than CD38 and ZAP-70. The authors concluded that CD49d expression and IGHV gene mutational status may be the strongest predictors of Overall Survival and Treatment Free Survival in patients with CLL and should be a part of routine baseline testing at the time of diagnosis. Bulian P, Shanafelt TD, Fegan C, et al. J Clin Oncol 2014;32:897-904
Retrospective studies have suggested that patients with CLL whose leukemic cells have clonotypically rearranged immunoglobulin genes in germline configuration (Unmutated IGHV gene) demonstrated more aggressive disease and shorter survival time compared to those patients with somatic hypermutations in their IGHV genes (Mutated IGHV gene). Expression of two flow cytometry based biomarkers, CD38 (surface marker) and ZAP-70 (intracytoplasmic protein), have been associated with poor outcomes. As we learn more about the pathobiology of CLL, it is becoming clear that survival of CLL cells is dependent not only on their intracellular defects but also on the microenvironment. CD49d, an integrin, is a surface molecule, detected by flow cytometry. CD49d expression promotes microenvironment mediated proliferation of CLL cells and has been associated with shortened survival. The authors conducted this multicenter analysis to evaluate the prognostic utility of CD49d in CLL, in comparison with CD38 and ZAP-70. The authors analysed the data of 2972 patients from 9 clinical trials. All these studies had data on CD49d expression of CLL cells by flow cytometry and reported the association between CD49d expression and Overall survival and/or Treatment Free Survival and/or Progression Free Survival. Patients with 30% or more of CLL cells expressing CD49d were considered CD49d positive. In this pooled analysis, CD49d positive patients had a significantly lower Overall Survival both at 5 years (87% vs 94%) and 10 years (62% vs 84%) compared with CD49d negative patients (P<0.001). Further, CD49d positive patients more likely required treatment, suggesting that these patients had a lower probability of remaining treatment free at both 5 years (42% vs 68%) and 10 years (24% vs 50%), compared with CD49d negative patients. When other variables were taken into consideration, CD49d was the only flow cytometry based marker which independently predicted Overall Survival with greater prognostic relevance than CD38 and ZAP-70. The authors concluded that CD49d expression and IGHV gene mutational status may be the strongest predictors of Overall Survival and Treatment Free Survival in patients with CLL and should be a part of routine baseline testing at the time of diagnosis. Bulian P, Shanafelt TD, Fegan C, et al. J Clin Oncol 2014;32:897-904

