SUMMARY: ColoRectal Cancer (CRC) is the third most common cancer diagnosed in both men and women in the United States. The American Cancer Society estimates that approximately 135,000 new cases of ColoRectal Cancer will be diagnosed in the United States in 2016 and over 49,000 patients are expected to die of the disease. The role of adjuvant chemotherapy in patients with Stage III ColoRectalCancer (CRC) has been well established, with improvement in Disease Free Survival (DFS) and Overall Survival (OS). However, not all patients equally benefit from this therapy. Patients with MSI (Micro Satellite Instability) tumor phenotype have better survival when cancer is at an earlier stage although this beneficial effect in Stage III colon cancer remains unclear.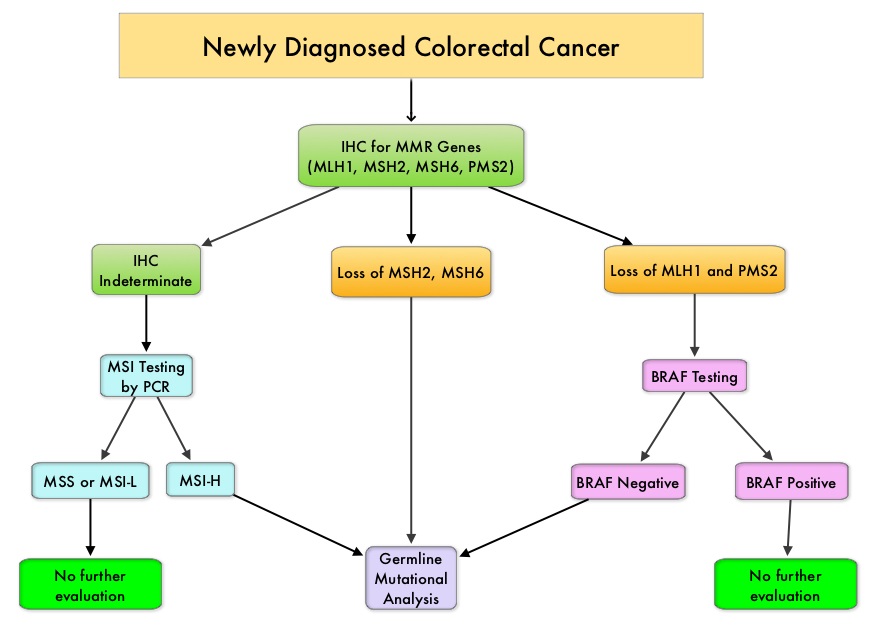
The DNA MisMatchRepair (MMR) system is responsible for molecular surveillance and works as an editing tool that identifies errors within the microsatellite regions of DNA and removes them. Defective MMR system leads to MSI (Micro Satellite Instability) and hypermutation, triggering an enhanced antitumor immune response. MSI (Micro Satellite Instability) is therefore a hallmark of defective/deficient DNA MisMatchRepair (MMR) system and occurs in 15% of all colorectal cancers. Defective MisMatchRepair can be a sporadic or heritable event. Approximately 65% of the MSI tumors are sporadic and when sporadic, the DNA MisMatchRepair gene is MLH1. Defective MisMatchRepair can also manifest as a germline mutation occurring in 1 of the 4 MisMatchRepair genes which include MLH1, MSH2, MSH6, PMS2. This produces Lynch Syndrome (Hereditary Nonpolyposis Colorectal Carcinoma – HNPCC), an autosomal dominant disorder and is the most common form of hereditary colon cancer, accounting for 35% of the MSI colorectal cancers. MSI tumors tend to have better outcomes and this has been attributed to the abundance of tumor infiltrating lymphocytes in these tumors from increase immunogenicity. These tumors are susceptible to PD-1 blockade and respond to treatment with checkpoint inhibitors such as Pembrolizumab (N Engl J Med 372:2509-2520, 2015).
MSI (Micro Satellite Instability) testing is performed using a PCR based assay and MSI-High refers to instability at 2 or more of the 5 mononucleotide repeat markers and MSI-Low refers to instability at 1 of the 5 markers. Patients are considered Micro Satellite Stable (MSS) if no instability occurs. MSI-L and MSS are grouped together because MSI-L tumors are uncommon and behave similar to MSS tumors. Tumors considered MSI-H have deficiency of one or more of the DNA MisMatchRepair genes. MMR gene deficiency can be detected by ImmunoHistoChemistry (IHC). MLH1 gene is often lost in association with PMS2.
Patients with stage IV colorectal cancer are now routinely analyzed for extended RAS and BRAF mutations because KRAS mutations are predictive of resistance to EGFR targeted therapy and BRAF V600E is recognized as a marker of poor prognosis in this patient group. BRAF mutations occur in approximately 45% of patients with sporadic colorectal cancer with MSI but not seen in patients with Lynch syndrome. The prognostic effect of these mutations in early stage disease has however remained controversial. This publication is a Post Hoc Analysis of the PETACC-8 study, a randomized phase III trial, in which patients with resected Stage III colon cancer received treatment with adjuvant FOLFOX with or without Cetuximab. The authors in this publication examined the prognostic effect of BRAF and KRAS mutations in this patient population, as it relates to MSI of the tumor.
The PETACC-8 trial enrolled 2559 patients with surgically resected colon cancer, treated with adjuvant FOLFOX chemotherapy regimen. The median age was 60 years. MisMatch Repair, BRAF V600E, and KRAS exon 2 mutational status, were determined on tumor blocks that were collected prospectively from the enrolled patients. MSI phenotype was noted in 9.9% (N=177), KRAS mutations in 33.1% (N=588) and BRAF V600E mutations in 9% (N=148) of the patients. The primary end point was Disease Free Survival (DFS) and Overall Survival (OS), as it relates to these mutations.
In multivariate analysis, MSI and BRAF V600E mutations for DFS were not prognostic, whereas KRAS mutation was associated with significantly shorter DFS (P<0.001) and OS (P=0.008). The subgroup analysis showed that in patients with Micro Satellite Stable (MSS) tumors, DFS and OS was inferior among those with KRAS and BRAF V600E mutation and were independently associated with worse clinical outcomes. In patients with MSI tumors, KRAS status was not prognostic, whereas BRAF V600E mutation was associated with significantly longer DFS (P=0.04), but not OS (P=0.08).
The authors based on this large analysis of patients with Stage III colon cancer receiving FOFOX adjuvant chemotherapy, concluded that BRAF V600E and KRAS mutations were significantly associated with shorter DFS and OS in patients with Micro Satellite Stable (MSS) tumors, but not in patients with MSI tumors. Prognostic Effect of BRAF and KRAS Mutations in Patients With Stage III Colon Cancer Treated With Leucovorin, Fluorouracil, and Oxaliplatin With or Without Cetuximab. A Post Hoc Analysis of the PETACC-8 Trial. Taieb J, Zaanan A, Le Malicot, et al. JAMA Oncol. 2016;2:643-653.

