SUMMARY: ColoRectal Cancer (CRC) is the third most common cancer and third leading cause of cancer-related deaths in both men and women in the United States. The American Cancer Society estimates that approximately 140,250 new cases of ColoRectal Cancer will be diagnosed in the United States in 2018 and over 50,630 patients are expected to die of the disease. The lifetime risk of colorectal cancer is 4.2% (1 in 24) in women and 4.5% (1 in 22) in men.
Vitamin D is known for its role in maintaining bone health and there is a growing body of evidence suggesting that Vitamin D has colon cancer preventing properties and may induce antitumor immunity. A study by Song and colleagues (Gut. 2015;64:260-271) showed that high plasma level 25-Hydroxy Vitamin D [25(OH)D] was associated with lower risk of colorectal cancer with intense immune reaction, supporting that vitamin D through tumor-host interaction may play a role in cancer immunoprevention. There also appears to be a strong association between plasma 25(OH)D level and colorectal cancer (CRC) specific mortality, with better outcomes in CRC patients with higher plasma levels of 25(OH)D, treated with a combination of chemotherapy and biologic agents. However the plasma concentrations of 25(OH)D that minimize colorectal cancer risk are unknown and even though epidemiological studies suggest a protective role for vitamin D in colorectal carcinogenesis, the evidence has been inconclusive. The current recommendations regarding vitamin D intake are based only on bone health. Sources of vitamin D include fatty fish like salmon, tuna and mackerel, foods fortified with vitamin D like some dairy products, cereals and orange juice as well as egg yolks. It is recommended that vitamin D be obtained through diet whenever possible rather than sun exposure, because of the risk of skin cancer with excessive UV radiation.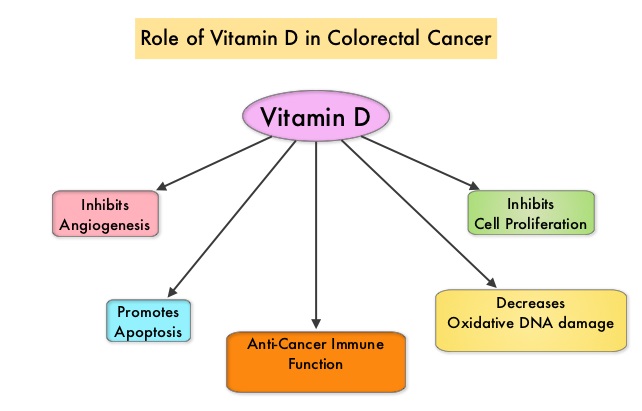
The Institute of Medicine defines vitamin D deficiency as plasma 25(OH)D level of less than 50 nmol/L and the plasma 25(OH)D threshold for fracture prevention is 75 nmol/L. All adults aged 50-70 years and more than 70 years will require at least 600 and 800 IU (15-20 μg) of vitamin D3 per day, respectively, for optimal bone health and muscle function. However, to raise the plasma level of 25(OH)D above 75 nmol/L, individuals will require at least 1500-2000 IU (37.5–50 μg) per day of supplemental vitamin D. Doses of up to 10 000 IU (250 μg) per day have been proven to be safe.
This present study was conducted to address inconsistencies in prior studies, on the protective role for vitamin D in colorectal cancer, and to investigate associations in population subgroups. The authors analyzed participant-level data, collected before colorectal cancer diagnosis, from 17 prospective cohorts which included 5706 colorectal cancer cases and 7107 control participants, from the US, Europe, and Asia, with a wide range of plasma 25(OH)D concentrations. A single, widely accepted assay and laboratory was used for new plasma 25(OH)D measurements, and calibration of previously measured plasma 25(OH)D. This calibration approach enabled the authors to systematically explore risk, utilizing the same assay, over the broad range of vitamin D levels seen internationally.
It was noted that compared to participants with plasma 25(OH)D concentrations sufficient for bone health (50-62.5 nmol/L), those with deficient 25(OH)D levels (less than 30 nmol/L) had a 31% higher risk of colorectal cancer during follow-up, which averaged 5.5 years. In contrast, individuals with plasma 25(OH)D levels above sufficiency for bone health, (75 to less than 87.5 nmol/L) had 19% lower risk and among those with plasma 25(OH)D levels 87.5 to less than 100 nmol/L, the risk of developing colorectal cancer was even lower at 27%. The risk however, did not continue to decline at plasma 25(OH)D levels of 100 nmol/L or greater. The protective association of high levels of plasma 25(OH)D persisted even after adjusting for known colorectal cancer risk factors such as Body Mass Index, physical activity, and other risk factors, and was seen in all subgroups examined. The protective association was more significant in women than men at plasma 25(OH)D levels above bone health sufficiency. For each 25 nmol/L increment in plasma 25(OH)D levels, colorectal cancer risk was 19% lower in women and 7% lower in men.
It was concluded that higher plasma 25(OH)D levels (75-100 nmol/L) was associated with a statistically significant lower colorectal cancer risk in women and non-statistically significant lower risk in men. This study suggested that the optimal plasma 25(OH)D level concentrations for colorectal cancer risk reduction appear higher than the levels recommended for bone health. Circulating Vitamin D and Colorectal Cancer Risk: An International Pooling Project of 17 Cohorts. McCullough ML, Zoltick ES, Weinstein SJ, et al. JNCI: Journal of the National Cancer Institute, https://doi.org/10.1093/jnci/djy087. Published: 14 June 2018.

