SUMMARY: The FDA on July 20, 2018, approved TIBSOVO® (Ivosidenib) for adult patients with relapsed or refractory Acute Myeloid Leukemia (AML) with a susceptible Isocitrate DeHydrogenase-1 (IDH1) mutation, as detected by an FDA-approved test. The American Cancer Society estimates that in 2018, 19,520 new cases of Acute Myeloid Leukemia (AML) will be diagnosed in the United States and 10,670 patients will die of the disease. AML can be considered as a group of heterogeneous diseases with different clinical behavior and outcomes. Cytogenetic analysis has been part of routine evaluation when caring for patients with AML. By predicting resistance to therapy, tumor cytogenetics will stratify patients, based on risk and help manage them accordingly. Even though cytotoxic chemotherapy may lead to long term remission and cure in a minority of patients with favorable cytogenetics, patients with high risk features such as unfavorable cytogenetics, molecular abnormalities, prior myelodysplasia and advanced age, have poor outcomes with conventional chemotherapy alone.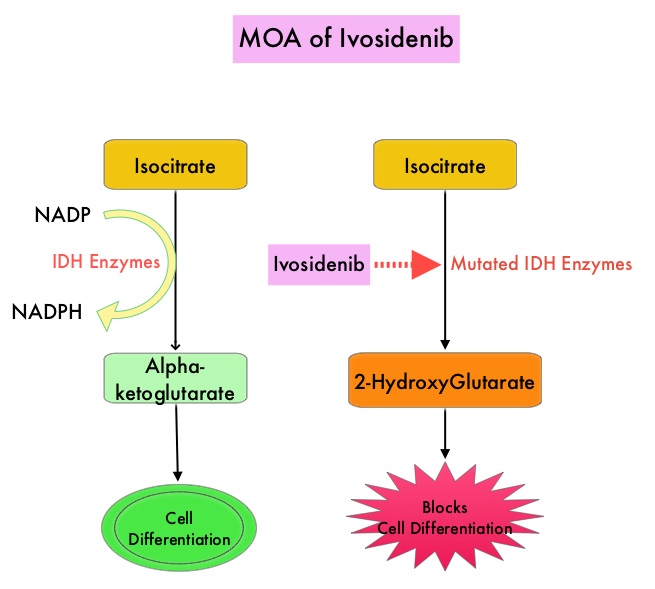
Isocitrate DeHydrogenase (IDH) is a metabolic enzyme that helps generate energy from glucose and other metabolites, by catalyzing the conversion of Isocitrate to Alpha-Ketoglutarate. Alpha-ketoglutarate is required to properly regulate DNA and histone methylation, which in turn is important for gene expression and cellular differentiation. IDH mutations lead to aberrant DNA methylation and altered gene expression thereby preventing cellular differentiation, with resulting immature undifferentiated cells. IDH mutations can thus promote leukemogenesis in Acute Myeloid Leukemia and tumorigenesis in solid tumors and can result in inferior outcomes. There are three isoforms of IDH. IDH1 is mainly found in the cytoplasm, as well as in peroxisomes, whereas IDH2 and IDH3 are found in the mitochondria, and are a part of the Krebs cycle. Approximately 20% of patients with AML, 70% of patients with Low-grade Glioma and secondary Glioblastoma, 50% of patients with Chondrosarcoma, 20% of patients with Intrahepatic cholangiocarcinoma, 30% of patients with Angioimmunoblastic T-cell lymphoma and 8% of patients with Myelodysplastic syndromes/Myeloproliferative neoplasms, are associated with IDH mutations.
TIBSOVO® is an oral, targeted, small-molecule inhibitor of mutant IDH1. IDHIFA® (Enasidenib), an oral, selective, small molecule inhibitor of mutated IDH2 protein was approved in the United States in August 2017 for adult patients with relapsed or refractory AML with an IDH2 mutation. The Complete Remission (CR) rate with the currently available non-targeted therapies for patients with relapsed or refractory AML is 15% or less and the median Overall Survival is less than 4 months, with 30-day mortality of approximately 15% and 60-day mortality of approximately 30%.
The approval of TIBSOVO® was based on an open-label, single arm, multicenter clinical trial that included 174 adult patients with relapsed or refractory AML with an IDH1 mutation. IDH1 mutations were confirmed by the Abbott RealTime® IDH1 assay, the FDA-approved test for selection of patients with AML for treatment with TIBSOVO®. TIBSOVO® was given orally at a starting dose of 500 mg daily until disease progression, unacceptable toxicity, or hematopoietic stem cell transplantation. The median treatment duration was 4.1 months. Twenty one of the 174 patients (12%) received a Stem Cell Transplant following treatment with TIBSOVO®. The median patient age was 67 years, patients had a median number of 2 prior therapies, 87% of the patients had intermediate or poor cytogenetic risk status, 33% had secondary AML and 59% were refractory to their previous therapy. The Primary endpoint was the combined rate of Complete Remission (CR) plus Complete Remission with partial hematologic recovery (CRh) and the rate of conversion from transfusion dependence to independence. CRh was defined as less than 5% of blasts in the bone marrow, no evidence of disease, and partial recovery of peripheral blood counts (platelets more than 50,000/μl and ANC more than 500/μl)
The use of TIBSOVO® was associated with a CR plus CRh rate of 32.8%. The median time to response was 2 months and the median response duration was 8.2 months. The CR and CRh rates were 24.7% and 8.0% respectively. Among the 110 patients who were dependent on Red Blood Cell and/or platelet transfusions at baseline, 37.3% became transfusion independent during any 56-day post-baseline period. Of the 64 patients who were independent of both RBC and platelet transfusions at baseline, 59.4% remained transfusion independent during any 56-day post-baseline period. The most common adverse reactions were fatigue, nausea, diarrhea, rash, pyrexia, arthralgia, leukocytosis and QT prolongation. One effect of the IDH inhibitors are induction of differentiation of the malignant cells, and in 10-20% of patients, a clinical syndrome known as the IDH differentiation syndrome can occur. The IDH differentiation syndrome should be promptly managed by dose interruption and treatment with glucocorticoids, oral hydroxyurea, or both.
It was concluded that in patients with advanced IDH1-mutated relapsed or refractory AML, TIBSOVO® fills an unmet need, with durable molecular remissions and reduction in the need for transfusion support. Durable Remissions with Ivosidenib in IDH1-Mutated Relapsed or Refractory AML. DiNardo CD, Stein EM, de Botton S, et al. N Engl J Med 2018; 378:2386-2398

