SUMMARY: The Center for Disease Control and Prevention (CDC) estimates that approximately 1-2 per 1000 individuals develop Deep Vein Thrombosis/Pulmonary Embolism (PE) each year in the United States, resulting in 60,000 – 100,000 deaths. VTE is the third leading cause of cardiovascular mortality with a mortality rate of up to 25% in those with untreated acute Pulmonary Embolism. The American College of Physicians in 2015 released pulmonary embolism guidelines after noting that there has been a dramatic increase in the testing for suspected acute Pulmonary Embolism (PE). 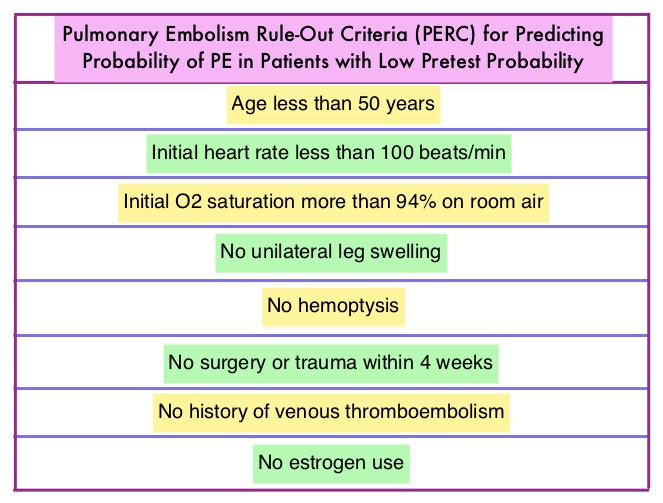 There has also been an overuse of CT imaging and plasma d-Dimer measurement, without improvement in care, but rather harming the patient and increasing expenditure. The validated clinical decision tools, in addition to physician’s clinical judgment include the Wells and Geneva Scoring System. The PERC (see table) criteria includes 8 elements, which if absent in low risk patients rules out PE. These practice guidelines were developed to provide practical advice, based on the best available evidence.
There has also been an overuse of CT imaging and plasma d-Dimer measurement, without improvement in care, but rather harming the patient and increasing expenditure. The validated clinical decision tools, in addition to physician’s clinical judgment include the Wells and Geneva Scoring System. The PERC (see table) criteria includes 8 elements, which if absent in low risk patients rules out PE. These practice guidelines were developed to provide practical advice, based on the best available evidence.
Best Practice Advice 1: Clinicians should use validated clinical prediction tools to estimate pretest probability, in patients in whom acute PE is being considered. These clinical decision tools include physician’s clinical judgment as well as Wells and Geneva Scoring System.
Best Practice Advice 2: The PERC (see table) criteria includes 8 elements. Clinicians should not obtain d-Dimer measurements or imaging studies in patients with a low pretest probability of PE and who meet all Pulmonary Embolism Rule-Out (PERC) Criteria.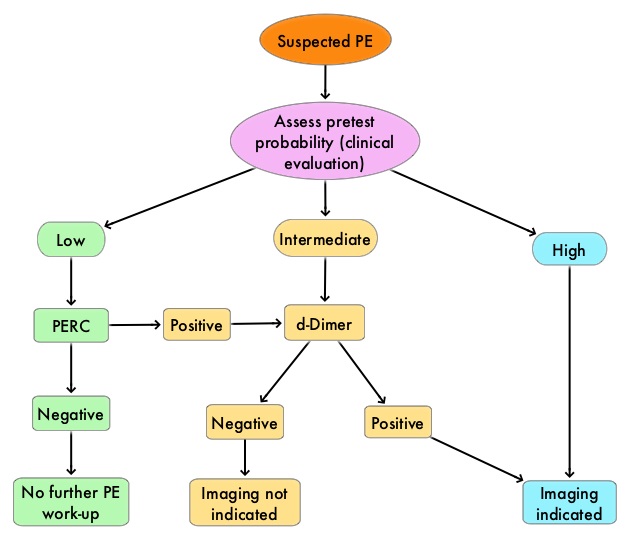
Best Practice Advice 3: For patients who have an intermediate pretest probability of PE or in patients with low pretest probability of PE who do not meet all PERC Criteria, clinicians should obtain a high-sensitivity d-Dimer measurement as the initial diagnostic test in patients. Clinicians should not use imaging studies as the initial test in patients who have a low or intermediate pretest probability of PE.
Best Practice Advice 4: Clinicians should use age-adjusted d-Dimer thresholds (age × 10 ng/mL rather than a generic 500 ng/mL) in patients older than 50 years because, normal d-Dimer levels increase with age.
Best Practice Advice 5: Clinicians should not obtain any imaging studies in patients with a d-Dimer level below the age-adjusted cutoff.
Best Practice Advice 6: Clinicians should obtain imaging with CT pulmonary angiography (CTPA) in patients with high pretest probability of PE. Clinicians should reserve ventilation–perfusion scans for patients who have a contraindication to CTPA or if CTPA is not available. Clinicians should not obtain a d-Dimer measurement in patients with a high pretest probability of PE because, a negative d-Dimer test will not preclude the need for imaging.
Evaluation of Patients with Suspected Acute Pulmonary Embolism: Best Practice Advice From the Clinical Guidelines Committee of the American College of Physicians. Raja AS, Greenberg JO, Qaseem A, et al. Ann Intern Med. 2015;163:701-711

