SUMMARY: Stereotactic RadioSurgery (SRS) is a non-surgical procedure that allows delivery of significantly higher doses of precisely focused radiation to the tumor, compared to conventional radiation therapy, with less collateral damage to the surrounding normal tissue. The technologies used for SRS include GAMMA KNIFE® which uses highly focused gamma rays, Proton Beam therapy which uses ionized hydrogen or Protons, Linear Accelerator (LINAC) and CYBER KNIFE® which use Photons, to target the tumor tissue. Stereotactic Body Radiation Therapy (SBRT) refers to stereotactically guided radiation therapy delivered over several days. Because SBRT is fractionated and is offered in three precise treatments, the short-and long-term side effects of radiation therapy are decreased and may allow higher total dosage to be given.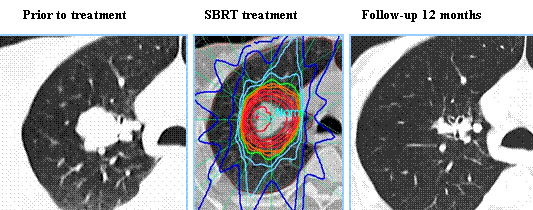
SBRT is a viable option for elderly and frail patients and those with comorbidities or those who decline surgery. Two studies presented at the 56th Annual Meeting of the American Society for Radiation Oncology (ASTRO) have provided convincing evidence in favor of SBRT in patients with inoperable early-stage lung cancer and for patients with oligometastatic stage IV Non Small Cell Lung Cancer (NSCLC). RTOG 0236 is a phase II trial in which 59 frail, elderly patients with early stage, medically inoperable Stage I Non Small Cell Lung Cancer received SBRT in three fractions of 18 Gy (total of 54 Gy) over a period of 10 days to 2 weeks. The median age was 72 years and these patients had multiple comorbidities that precluded them from curative surgery. The primary end point was 2-year actuarial primary tumor control. Secondary end points included Disease Free Survival (i.e., primary tumor, involved lobe, regional, and disseminated recurrence), treatment-related toxicity and Overall Survival. At 5 years, the Disease Free Survival and Overall Survival were 26% and 40%, respectively and the median Overall Survival was 4 years. The 5-year primary tumor and involved lobe (local) failure rate was 20%, local-regional failure rate was 38% and disseminated failure rate was 31%. In a second study, Ashworth and colleagues reported the individual patient data meta-analysis, which included 757 patients diagnosed with stage IV NSCLC at 20 cancer centers worldwide. All patients had 1-5 synchronous or metachronous metastases treated with surgical metastectomy, SBRT, or radical external beam radiation therapy and the primary tumor was treated aggressively with a curative intent. The 1-year Overall Survival (OS) was 70.2% and 5-year Overall Survival was 29.4%. The authors were able to develop a risk stratification model for survival, to help identify which patients would be the best candidates for SBRT or surgery. They noted that patients with metachronous metastases had a 5-year Overall Survival of 48% and were considered low risk, those with synchronous metastases and negative nodes had a 5-year OS of 36% and were considered intermediate risk and patients with synchronous metastases and positive nodes were considered high risk and had a 5-year overall survival of 14%.
Taken together, these two studies have demonstrated that SBRT improves Overall Survival in elderly frail patients with medically inoperable early stage Lung Cancer and SBRT also improves Overall survival in patients Stage IV Non Small Cell Lung Cancer, with metachronous metastases without nodal involvement. A multidisciplinary team approach is strongly recommended, as treatment decisions are made for the latter group.
1)Long-term Results of RTOG 0236: A Phase II Trial of Stereotactic Body Radiation Therapy (SBRT) in the Treatment of Patients with Medically Inoperable Stage I Non-Small Cell Lung Cancer. Timmerman RD, Hu C, Michalski J, et al. DOI:http://dx.doi.org/10.1016/j.ijrobp.2014.05.135
2)An Individual Patient Data Meta-Analysis of Outcomes and Prognostic Factors After Treatment of Oligometastatic Non-Small Cell Lung Cancer. Ashworth A, Senan S, Palma DA, et al. DOI: http://dx.doi.org/10.1016/j.ijrobp.2014.08.028

